Imagine, for a devastating injury such as a knee anterior cruciate ligament (ACL) tear or shoulder rotator cuff tendon tear, that your physician could inject a mixture of blood taken from your body that could improve your ability to heal these injuries. What you may be imagining is now a reality. This reality, called biologic augmentation for orthopedic healing - or orthobiologics - is bringing exciting results for both physicians and patients.
What are Orthobiologics?
Orthobiologics are natural substances that orthopedic surgeons use to enhance the body’s ability to heal more quickly. They can be made from substances including platelet rich plasma and bone marrow aspirates of autologous stem cells. Using these can enhance the body’s ability to heal injuries including broken bones and injured muscles, tendons, and ligaments.
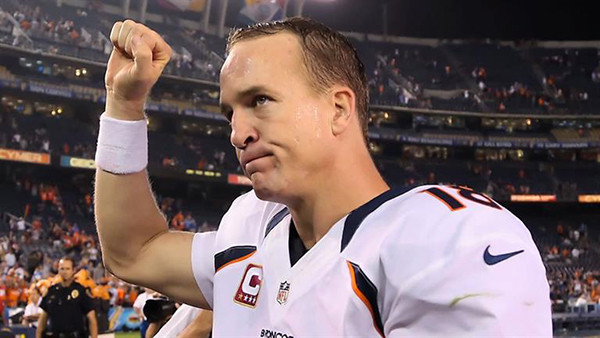
You may have heard about celebrities and athletes traveling the globe in search of treatment with PRP or stem cells. In fact, recent Super Bowl winner, Peyton Manning, received stem cell treatments in his injured neck in 2011 before a subsequent neck fusion surgery.
But even though treatments have been successfully performed, there are still many questions regarding the use of orthobiologics, including:
- What is platelet-rich plasma (PRP) and what are its benefits?
- How does PRP work and is it for me?
- What are growth factors and where do they come from?
- What are stem cells and where do they come from?
- What conditions or diseases can PRP and stem cells be used for?
- What is the evidence to support their use to treat orthopedic injuries?
We’ll attempt to address these questions in this multi-part informational series, starting with a focus on PRP.
What is Platelet-Rich Plasma (PRP)?
Simply put, PRP is blood plasma that has been enriched with platelets. Blood is a liquid mixture of plasma, red blood cells, white blood cells, and platelets. Platelets are primarily involved in blood clotting but they also contain hundreds of small packages (granules) of growth factors and cytokines which help control processes of healing. Many growth factors are contained in these granules including insulin like-growth factor-1 (IGF-1), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and a host of others. The signals from these growth factors and cytokines control processes such as building new connective tissue, creating new blood vessels, recruiting other cells to help healing, and controlling inflammation.
When plasma from blood contains an increased concentration of platelets, then it is considered platelet-rich plasma (PRP). Creation of PRP occurs by centrifuging (spinning) a sample of blood in order to concentrate the number of platelets into a small volume. Typically, the concentration of platelets is three to five times the concentration found in blood. Centrifuging the blood enables the separation of components of blood - the plasma, red blood cells, white blood cells, and platelets - based on size. Concentrating platelets in a small volume of plasma and separating out the red and white blood cells leads to the creation of a powerful healing product with multiple growth factors and cytokines - PRP.
PRP has been employed to help healing of multiple orthopedic ailments. Generally, its use can be grouped into one of four categories of orthopedic injuries: chronic tendon injuries (i.e. tennis elbow), acute soft tissue injuries (hamstring strains/tears), arthritis, and surgical augmentation. Some conditions such as tennis elbow (lateral epicondylitis) and knee osteoarthritis have been more rigorously tested in multiple clinical trials where as other conditions such as fractures, rotator cuff tears, patellar tendonitis, Achilles tendonitis, plantar fasciitis, muscular strains/tears, shoulder osteoarthritis, hip osteoarthritis, and many other conditions have been less rigorously tested. Nevertheless, the hope that PRP can help any orthopedic condition has captured the fascination of medical professionals, the media, and the general public.
What are the Benefits of PRP Therapy?
There are three standout benefits of PRP therapy. First, it is an autologous biologic product--meaning that it comes from the same individual that is receiving the treatment. It uses your body’s own natural healing ability (growth factors and cytokines) to promote healing and pain relief. Second, it is an injection and can be directed with ultrasound guidance or fluoroscopic guidance directly to the site of injury with minimal discomfort. Finally, it has the potential to return you to activity in a short time without surgery. This is beneficial in terms of not only shortened recovery, but also in terms of avoiding the high costs of surgery and missed time off work.
How Does PRP Work and Is it for Me?
PRP can be used as a nonsurgical treatment when other nonsurgical treatments have failed, and sometimes it is used during surgery as an adjunct to help speed healing. To prepare PRP, first a small volume of blood is drawn from the patient. The blood is then centrifuged to make PRP. There has been some controversy regarding the exact mixture/concentration of platelets, white blood cells, and growth factors that is necessary to treat certain conditions. In fact, the medical community and scientists are constantly refining the perfect formula of PRP to treat specific conditions such as tennis elbow or osteoarthritis.
Although there are many positives, PRP is not always the right choice for every patient. As with most new medical advances, PRP is still considered experimental by most insurance companies. Physicians are actively collecting data in a registry to track patients that receive PRP treatments, in order to provide data to show the safety and success rates of these treatments. To learn more about PRP to treat orthopedic injuries, please call or to schedule an appointment.
Please check back to read about our next topic, stem cells in orthopedics.